Enjoying a good night’s sleep and waking up feeling refreshed and energised will help you enjoy the things you love.
Treating your sleep apnea can empower you to sleep sounder, awake brighter and live a healthier life.
Apnea literally means “no breath” or “stopping breathing”. When you have sleep apnea, air stops flowing to your lungs for 10 seconds or longer – that is, you actually stop breathing.
This makes your blood oxygen level drop which in turn triggers your brain to wake you up just enough to take a breath.1 Then you fall back to sleep and the cycle begins again.
This can happen more than 30 times every hour and you may not even know it. As you can imagine, constantly being triggered back into breathing, hour after hour, night after night, can put a strain on your body. The next day you may feel tired and wrung out. Sleep apnea isn’t just an inconvenience. Left undiagnosed and untreated, it can have serious long-term effects on your health.2,3 It’s so common! 3 in 10 men and almost 1 in 5 women have sleep apnea.4

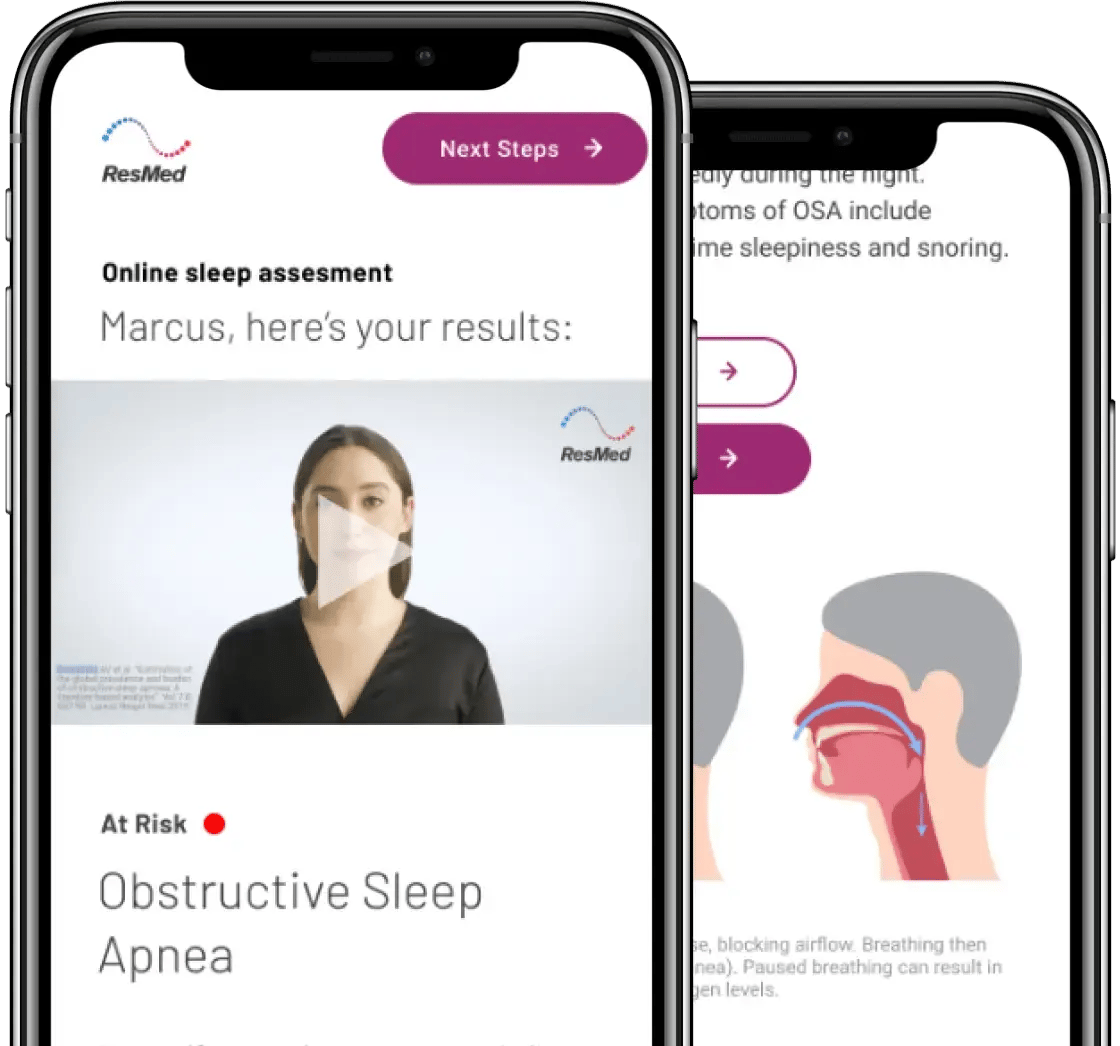
Obstructive sleep apnea is by far the most common type of sleep apnea.5 It happens when your upper airways become blocked or partially blocked when you sleep. The blockage is usually in your nose or throat. Common obstructive sleep apnea causes are:
Loud snoring, gasping for breath and daytime tiredness are common warning signs of obstructive sleep apnea, although some people with obstructive sleep apnea don’t snore much at all.


Central sleep apnea is more uncommon.5 It happens when your brain doesn’t tell your body to take a breath. Because central sleep apnea doesn’t cause much in the way of snoring, it often goes unnoticed.

If you have a mixture of obstructive sleep apnea and central sleep apnea, then you have mixed sleep apnea.
There are degrees of severity of sleep apnea. Sleep apnea is diagnosed as mild, moderate or severe depending on how many apnea events you have per hour. An event is when there is a complete or partial loss of breath for a minimum of 10 seconds. Complete loss of breath is called an apnea. Partial loss of breath is called a hypopnea. Sleep apnea can be diagnosed by taking a home sleep test.
The result of your sleep test gives you a number called an Apnea/Hypopnea Index (known as AHI). Your AHI number gives you (and your doctor) a guide to the best treatment options for you. Learn more about sleep apnea treatment.
In adults the most common cause of obstructive sleep apnea is obesity. Being overweight can add extra fat around the neck and airways. During sleep the throat and tongue muscles relax causing the airway to become blocked. But obesity is not the only cause - other factors are also associated with sleep apnea.
Learn more about what causes sleep apnea.
Central sleep apnea occurs when your brain doesn’t tell your body to take a breath. It’s normally associated with other conditions such as heart failure or stroke.7
If you have a family member who’s been diagnosed with sleep apnea, you’ll probably be concerned that you might also be at risk, especially if you snore. The risk of you having obstructive sleep apnea is about 50% higher if you have a parent, child or sibling with the condition.8 However, you can reduce your risk of sleep apnea in the future with some lifestyle changes.
Because you’re asleep when it happens, sleep apnea symptoms can go undetected. If you sleep with a partner, you may have been told that you snore, stop breathing or make gasping sounds in your sleep.
Daytime sleep apnea symptoms9,10 include:
Did you know, 3/10 men and 1/5 women have sleep apnea.1 Learn more about your sleep today, it only takes a few minutes.



Yes, sleep apnea is a dangerous condition that can lead to numerous health problems such as high blood pressure and diabetes if left untreated.
Untreated sleep apnea can also lead to daytime sleepiness, which makes you more prone to roadside and workplace accidents.
Many people have sleep apnea and don’t even know it. If you think that you may have symptoms of this disorder, then you may want to seek the advice of your doctor and/or have a sleep study done.
Studies have shown that obstructive sleep apnea can be hereditary, which means the condition can be passed on from one generation to another.13
Even though research has shown that there is a genetic component involved with obstructive sleep apnea, there is still no clarity on the specific genes that are involved with it.
There is currently no cure for sleep apnea, but there are several different options available for treating sleep apnea. Note that treatment options will vary depending on the type and severity of sleep apnea that is present.
Treatment options for obstructive sleep apnea include:
No, a deviated septum cannot cause sleep apnea, but it can increase the severity of sleep apnea present. If you have a deviated septum then your symptoms may be worse. You may also notice an increase in apnea events while you sleep.
Even though a deviated septum has not shown to be a direct cause of the condition it can be used to help identify that the condition is present in the first place.
If you are someone who has a deviated septum and believes it is affecting your sleep then it is recommended that you consult an ENT specialist to discuss the options that are available to you.
Yes, being overweight can cause sleep apnea. Obesity and excess weight is the most common cause of obstructive sleep apnea.
Asthma and sleep apnea are two conditions that often go hand-in-hand. It is important for people with asthma to be aware of the symptoms of sleep apnea to make sure they are getting the proper required treatment.
Source: Harrington, C. The Complete Guide to a Good Night's Sleep. Pan MacMillan Australia 2014
Source: Wolk R et al. Circulation 2003; 108: 9-12.
Source: Buchner NJ et al. Am J Respir Crit Care Med 2007; 176(12): 1274-1280.
Source: Peppard PE et al. Am J Epidemiol. 2013 (5.17).
Source: Morgenthaler TI et al. Complex sleep apnea syndrome: is it a unique clinical syndrome? Sleep 2006;29(9):1203-9.
Source: https://www.webmd.com/sleep-disorders/sleep-apnea/sleep-apnea-ahi-numbers accessed 24 June 2019
Source: https://www.mayoclinic.org/diseases-conditions/central-sleep-apnea/symptoms-causes/syc-20352109 accessed 2 July 2019.
Source: https://ghr.nlm.nih.gov/condition/obstructive-sleep-apnea#inheritance accessed 2 Aug 2019
Source: Palnitkar G, et al. Medicine Today 2012, 13(8):14-23.
Source: Wong SH, Ng BY. Singapore Med J. 2015 Jun;56(6):317-23.
Source: Appleton SL et al. Sleep Health 4 (2018) 13–19
Source: https://www.sleepfoundation.org/articles/women-and-sleep-apnea accessed 2 Aug 2019
Source: https://doi.org/10.5665/sleep.1366 accessed 23 June 2021