ResMed offers you intelligent non-invasive ventilation solutions that can help you tailor treatment to the unique and changing needs of your patients. From ventilators and masks to oxygen options and accessories, ResMed’s solutions work together to help patients breathe easier as they manage their condition.
Today, on World COPD Day, we are excited to share the results of the HOT-HMV trial presented at ERS, which show that HMV added to HOT can reduce by 51% the likelihood of readmissions to hospital or death over one year in hypercapnic COPD patients following an acute exacerbation of COPD.1 There are new prospects for better treatment of COPD—and better lives for patients.

Successful ventilation relies on improving gas exchange and reducing the work of breathing while keeping the patient comfortable. Maintaining patient-device synchrony and managing leak is critical to achieving this.
Ventilator asynchrony can cause significant discomfort, distress and poor clinical outcomes. One study estimates that 40% of non-invasive ventilation patients experience asynchrony in 10% or more of their breaths.1,2
A good device should help overcome this by:
Designed to identify changes to a patient’s breathing, where sensitivity to leak and patient–ventilator asynchrony is important, all our devices feature the following technologies to help you provide better clinical outcomes:
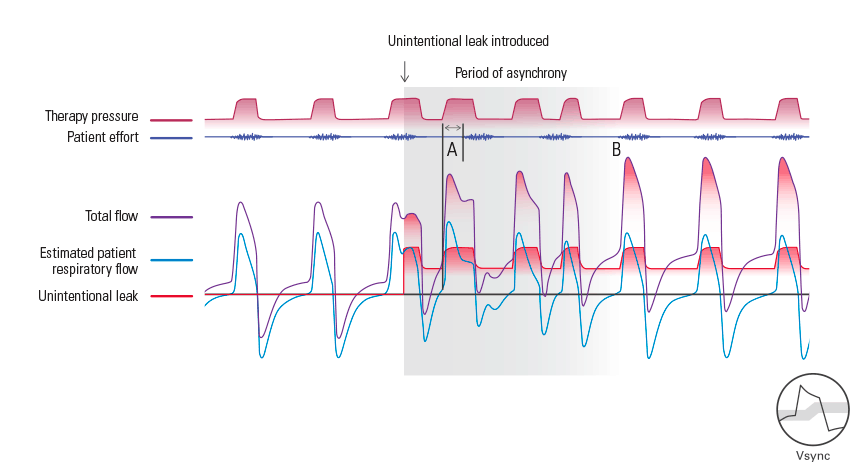
Acutely sensitive to a patient’s breathing, our Vsync algorithm rapidly compensates for any presence of leak by automatically adjusting the baseline flow. And because it can also accurately estimate respiratory flow and tidal volume, it is beneficial for circuits with intentional leak. All this is achieved while maintaining reliable triggering and cycling, and set pressures.
TiControl allows clinicians to limit the minimum and maximum amount of inspiratory time to suit a patient’s condition. For COPD patients, whose respiratory flow is restricted, and who have difficulties exhaling, a shortened Ti Max (maximum time a patient can spend in inspiration) can prevent late cycling to expiratory pressure, which helps provide a better match to the patient’s ideal inspiratory time.
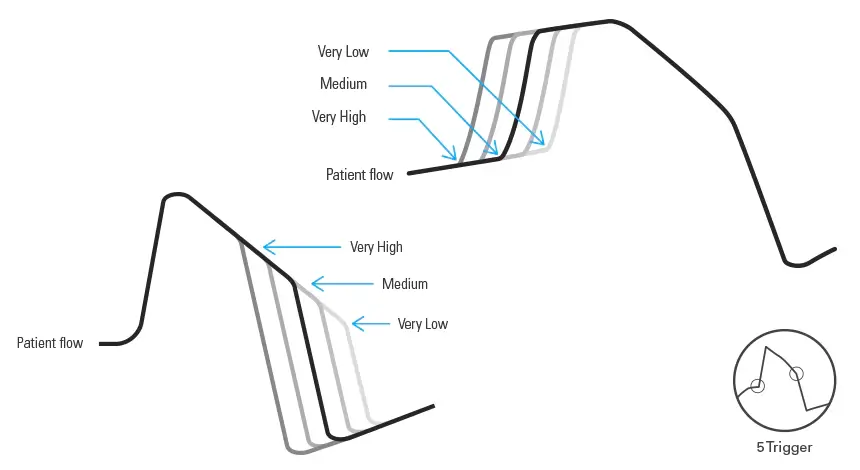
By determining the timing and level of effort at the beginning and end of each breath, you can fine-tune sensitivity settings to match a patient’s spontaneous breath cycle.
For Lumis™ and Astral™ ventilators, the default Medium setting will be appropriate in most cases.
Major therapy parameters can be pre-programmed in some of our ventilators to help you set up. (E.g. By choosing ‘Obstructive Lung’ from the Pathology Defaults for patients with COPD using a Stellar™ ventilator.)
However, having the option to fine-tune trigger and cycle sensitivities allows further customisation at the beginning and end of each inspiration.
This helps reduce the patient’s work of breathing, and optimise patient–ventilator synchrony.
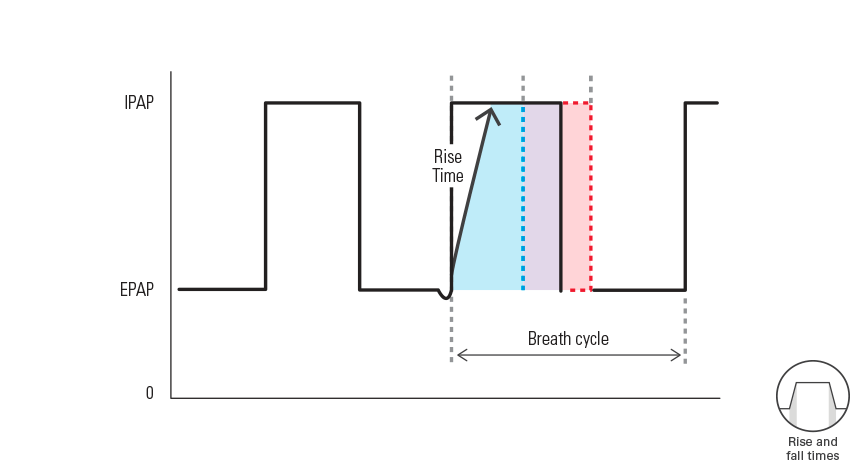
Rise time is the time it takes for the ventilator to reach the set inspiratory pressure after triggering; Fall time is the time it takes to reach the set expiratory pressure after cycling.
Rise and fall times can be tailored to suit different individuals and their conditions. Faster rise and fall times ensure rapid transitions, while slower times provide a more gradual transition.
For a COPD patient, a faster rise time setting can help the lungs fill quickly.
Traditional modes include:
CPAP mode—where a fixed pressure is delivered.
S (Spontaneous) mode—the device senses the patient’s breath and delivers IPAP in response to an increase in flow, and cycles into EPAP at the end of inspiration. The breath rate and respiratory pattern will be determined by the patient’s breathing.
ST (Spontaneous/Timed) or PS (Pressure Support) mode—the device augments any breath initiated by the patient, but will also supply additional breaths should the patient’s breath rate fall below the clinician's set ’backup’ breath rate.
T (Timed) mode—the fixed breath rate and fixed inspiration time set by the clinician are supplied regardless of patient effort.
PAC (Pressure Assist Control)—the inspiration time is pre-set in PAC mode. There is no spontaneous/flow cycling. The inspiration can be triggered by the patient when the respiratory rate is above a pre-set value, or time-triggered breaths will be delivered at the backup breath rate.
With the introduction of iVAPS mode, an intelligent back-up rate (iBR), and auto-adjusting AutoEPAP feature, we can help set a new standard in personalised and responsive ventilation for COPD patients. Together, we call these new technologies ‘IntelligentAir’.
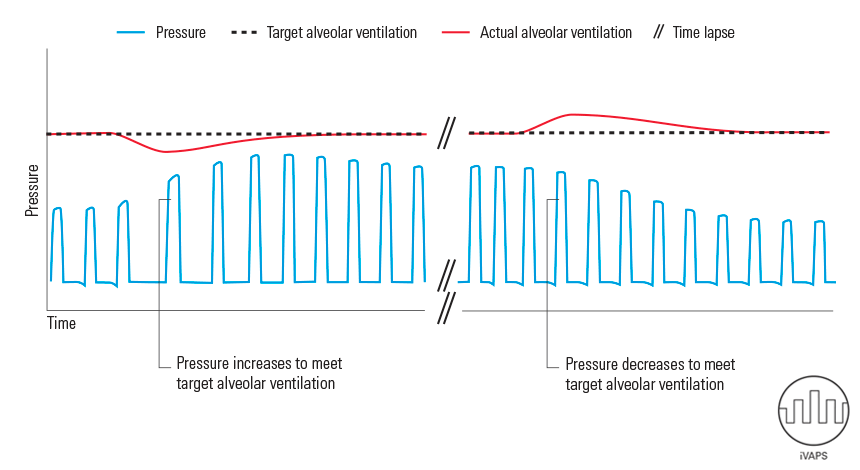
Targeting each patient’s unique alveolar ventilation, iVAPS mode auto-adjusts the pressure support to maintain that target, and stabilise the patient’s breathing.
iVAPS automatically adapts to the patient’s changing needs by constantly monitoring their actual ventilation and respiratory rate in relation to their target ventilation and respiratory rate.
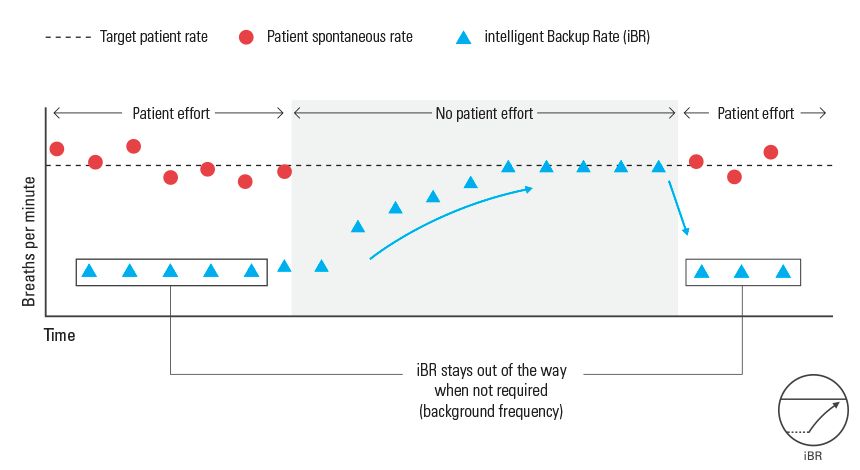
A feature of iVAPS, the intelligent Backup Rate (iBR) provides backup breaths only when needed, to allow maximum opportunity for spontaneous breathing.
Giving patients maximum opportunity to spontaneously trigger the ventilator, iBR shifts between two limits: the target patient rate, and its background frequency, which is two-thirds of the target rate.
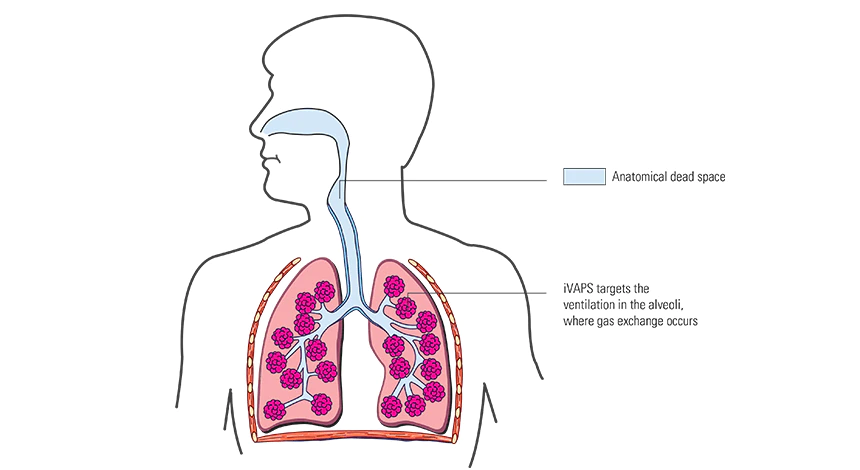
Some ventilation modes target tidal volume (or minute ventilation), without taking into account the anatomical dead space in the patient’s airways. What’s different about ResMed’s iVAPS mode is that it targets alveolar ventilation, which represents the most accurate measure of a patient’s lung and respiratory capacity.
Because iVAPS takes into account both tidal volume and respiratory rate, by targeting alveolar ventilation, the effect of respiratory rate variation on ventilatory support can be better controlled.
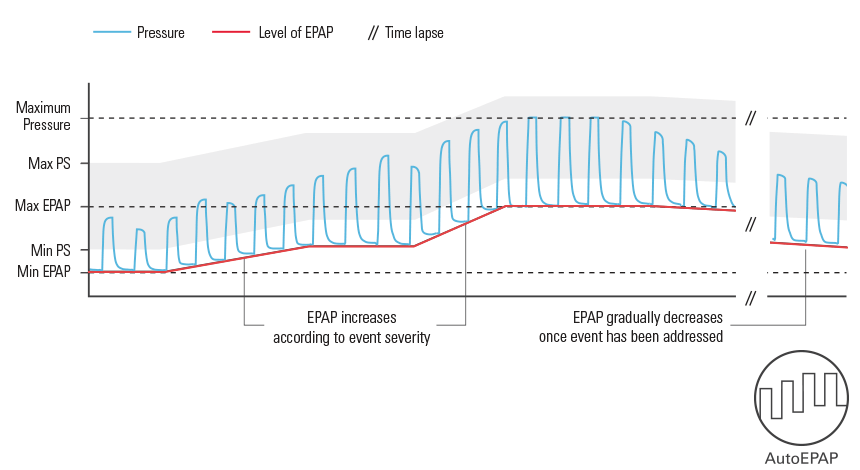
Complementing iVAPS, the optional AutoEPAP feature helps address partial and full obstructions to maintain upper airway patency.
AutoEPAP responds to upper airway obstructions by auto-adjusting expiratory pressure according to the severity of the event.
Our ventilators are designed with your COPD patients’ quality of life in mind. Patients can feel confident knowing that a ResMed ventilator will keep them supported as they continue with their daily lives in or out of the hospital and home.
ResMed’s non-invasive ventilators have simplicity built into their design, so it’s easy to set up, monitor and change therapy from the ventilator itself.
Easy to use in hospital as well as in patients’ homes, each of our ventilators features menu options that allow ‘low-touch’ therapy setup and adjustment.
A recent addition to the ResMed family, Lumis has an intuitive menu and small footprint. It can give COPD patients comfortable, personalised non-invasive ventilation with warmed, humidified air. Simple to set up and titrate, Lumis synchronises easily with the patient’s breathing. Lumis’ optional Ramp and Ramp down features help patients ease into and out of therapy.

Stellar is an invasive and non-invasive ventilator that is designed for versatility. It is suited for patients with changing ventilatory needs and progressive respiratory conditions, including COPD.

Astral is a life support ventilator, which can be used invasively or non-invasively for patients with more advanced needs who require round-the-clock therapy.

Building on 25 years of innovation, ResMed offers a wide range of mask types and sizes, designed for comfort, lightness and minimal face coverage. We also provide fitting instructions to help patients learn to fit their mask.
.png)
Personalised non-invasive ventilation made easy
.png)
Invasive and non-invasive ventilators designed for versatility
.png)
Portable life support ventilators to enrich life
.png)
Comfortable masks that fit a wide range of patients
PC-based clinical analysis and patient data management software
* World Health Organization. “Chronic respiratory diseases: Burden of COPD” Who.int. (accessed November 9, 2015)