Today, on World COPD Day, we are excited to share the results of the HOT-HMV trial presented at ERS, which show that HMV added to HOT can reduce by 51% the likelihood of readmissions to hospital or death over one year in hypercapnic COPD patients following an acute exacerbation of COPD.1 There are new prospects for better treatment of COPD—and better lives for patients.

Although there is currently no cure for COPD, treatments are available to help COPD patients with their day-to-day relief and long-term disease management.
The primary goals of treating COPD are to:
Given the progressive nature of COPD, treatment plans will vary depending on which stage of the disease your patients are facing.
Depending on the severity, patients experiencing acute exacerbations of COPD often suffer from increased airflow limitation, increased sputum production, airway inflammation, and respiratory insufficiency that can result in hypoxia, hypercapnia and respiratory acidosis.2
Recommended treatments for acute exacerbations may include:
While oxygen therapy is used to treat hypoxemic patients with impaired gas exchange or pulmonary failure, it does not adequately address carbon dioxide (CO2) retention in hypercapnic patients with ventilatory failure – but non-invasive ventilation can.3
The GOLD guidelines conclude that using non-invasive ventilation to manage acute exacerbations of COPD improves respiratory acidosis, decreases respiratory rate, reduces the severity of breathlessness, and lowers the rate of complications such as ventilator-associated pneumonia.1
Close to 20% of COPD patients who are hospitalised for an acute exacerbation are readmitted within 30 days.4 Another study found a readmission rate of 63% over a mean follow-up of 1.1 years.5
Using non-invasive ventilation to treat acute exacerbations in hospital has been shown to not only reduce readmission and lengths of stay, but also reduce the incidence of mortality and intubation.6 The prescribed use of non-invasive ventilation at home following COPD hospitalisation also suggests similar benefits.8
The long-term management of COPD seeks to optimise lung function, prevent exacerbations and slow disease progression. This often includes a self-management plan with multidisciplinary treatments tailored to suit individual patients.
Recommended treatments for better long-term outcomes may include:
With increasing burdens on our healthcare system, there has been interest shown for the use of non-invasive ventilation, not only when treating acute exacerbations, but also as a preventative therapy in the long-term management of COPD.2
A range of studies show encouraging findings when non-invasive ventilation is added to the treatment of COPD:

A recent clinical trial, the HOT-HMV study, indicates that home mechanical ventilation (HMV) combined with home oxygen therapy (HOT) can reduce hospital readmissions or death by 51% over a year in hypercapnic COPD patients after acute COPD exacerbation.
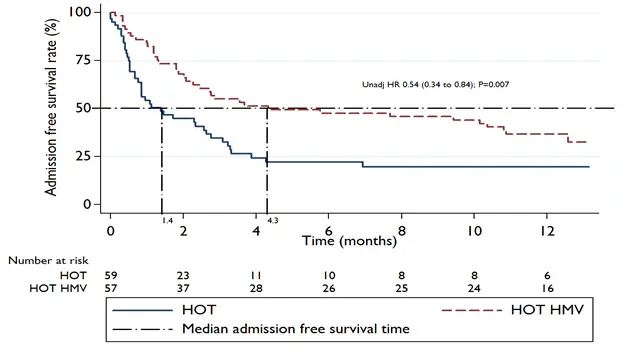
The results found an increase in patients’ median (hospital) admission-free survival from 1.4 months in the group receiving HOT only, to 4.3 months in the group receiving HOT plus HMV, with an adjusted hazard ratio of 0.49 (0.31-0.77); p=0.002.12
Admission free survival by treatment arm
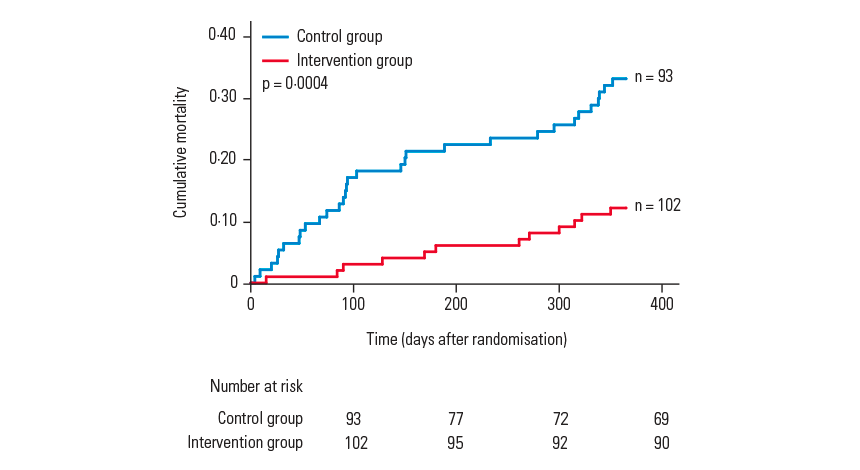
In a recent prospective, randomised controlled trial (Koehnlein et al. 2014), clinicians studied the use of home-based non-invasive ventilation compared to standard therapy for patients with stable hypercapnic COPD.
After a follow-up period of 12 months, the risk of mortality was 76% lower in the intervention group compared to the control group. Improvements were also reported for patient quality of life and exercise tolerance. 7
Reduction in mortality in hypercapnic COPD patients on non-invasive ventilation therapy
Kaplan-Meier estimate of cumulative all-cause mortality during the first year after randomisation. Adapted from Koehnlein et al. 2014.
A 2-year study (Duiverman et al. 2011) has demonstrated various clinical benefits for adding non-invasive ventilation to COPD treatment at home compared to pulmonary rehabilitation alone. The study reported improvements to the following outcomes, with benefits also increasing over time:
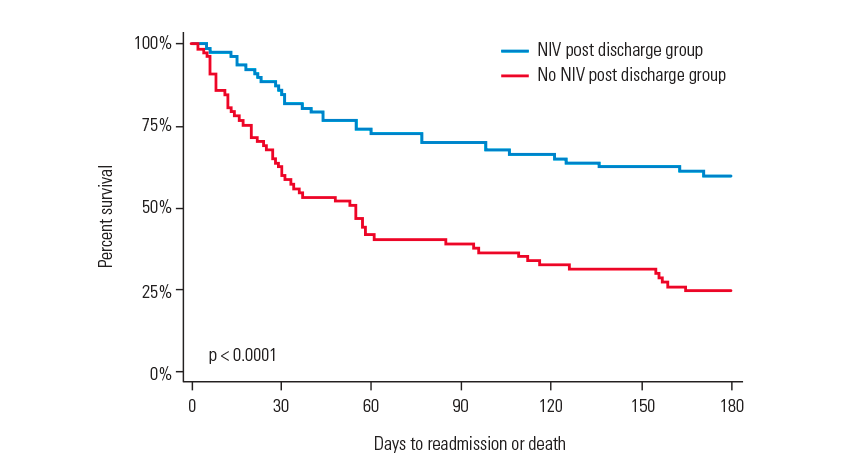
A retrospective study (Galli et al. 2014) assessed the outcomes for patients who were prescribed non-invasive ventilation at home compared to those who were not prescribed non-invasive ventilation.
Analysed data showed that patients who had been prescribed non-invasive ventilation at discharge were less likely to have been readmitted to hospital or readmitted with a stay in the intensive care unit.8
Effect of prior home non-invasive ventilation on event-free survival following readmission
Kaplan-Meier curves of event-free survival comparing patients who used home non-invasive ventilation versus patients who did not use home non-invasive ventilation. Adapted from Galli et al. 2014.
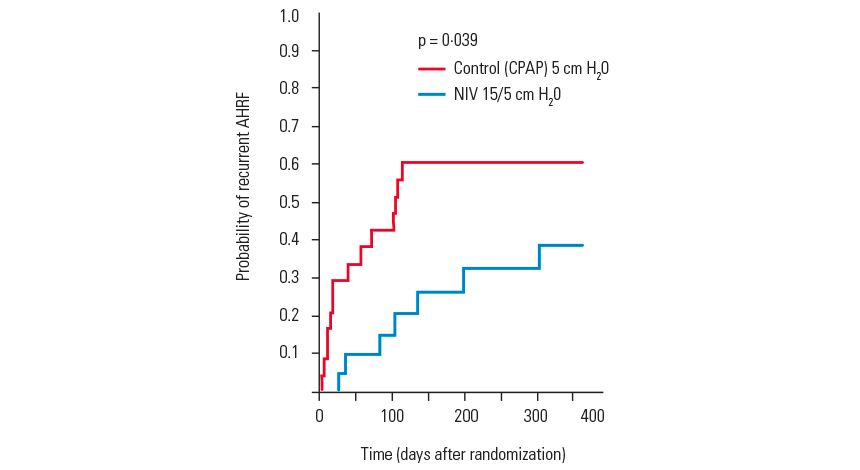
A pilot trial (Cheung et al. 2010 ) observed that COPD patients with acute hypercapnic respiratory failure (AHRF) were less likely to experience a recurrent severe exacerbation when treated with non-invasive ventilation compared to treatment with CPAP. The prevalence of patients developing recurrent AHRF in the non-invasive ventilation group compared to the CPAP group was 38.5% to 60.2% at 1 year.11
Effect of CPAP vs. non-invasive ventilation on patients with AHRF
Kaplan-Meier curves showing reduced rate of recurrent AHRF in COPD patients given home non-invasive ventilation compared with patients given CPAP. Adapted from Cheung et al. 2010.
With clinical evidence suggesting that non-invasive ventilation can improve quality of life and survival,7 and also help reduce the length of hospital stays and readmission rates,6 ResMed is working with respiratory physicians, healthcare systems and payors to increase awareness of non-invasive ventilation therapy, and has developed intelligent non-invasive ventilation solutions that are suitable for the treatment of COPD.
By choosing ResMed’s non-invasive solutions when treating COPD patients, you can provide an even more promising picture with every breath.
Global Initiative for Chronic Obstructive Lung Disease (GOLD). “Global Strategy for the Diagnosis, Management and Prevention of COPD, 2015.” Goldcopd.com. http://www.goldcopd.org/uploads/users/files/GOLD_Report_2015_Sept2.pdf (accessed November 9, 2015)
McKenzie DK et al. The COPDX Plan: Australian and New Zealand Guidelines for the management of Chronic Obstructive Pulmonary Disease 2003. Med J Aust. 2003;178 (6):S15-29.
Brill SE and Wedzicha JA. Oxygen therapy in acute exacerbations of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2014;9:1241–1252
Jencks SF et al. Rehospitalisations among patients in the Medicare fee-for-service program. New Engl J Med. 2009;360(14):1418-28.
Garcia-Aymerich J et al. Risk factors of re-admission to hospital for a COPD exacerbation: A prospective study.Thorax.2003;58:100–5.
Ram F et al. Non-invasive positive pressure ventilation for treatment of respiratory failure due to exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2004;CD004104.
Koehnlein T et al. Non-invasive positive pressure ventilation for the treatment of severe stable chronic obstructive pulmonary disease – A prospective, multicentre, randomized, controlled clinical trial. Lancet Respir Med. 2014;2:698-705.
Galp JA et al. Home non-invasive ventilation use following acute hypercapnic respiratory failure in COPD, Respir Med. 2014;108(5):722-8
Tsai CL. Comparative effectiveness of noninvasive ventilation vs invasive mechanical ventilation in chronic obstructive pulmonary disease patients with acute respiratory failure. J Hosp Med. 2013 Apr;8(4):165-72.
Duiverman ML et al. Two year home-based nocturnal noninvasive ventilation added to rehabilitation in chronic obstructive pulmonary disease. Respir Res. 2011;12(1):112.
Cheung AP et al. A pilot trial of non-invasive home ventilation after acidotic respiratory failure in chronic obstructive pulmonary disease. Int J Tuberc Lung Dis. 2010;14(5):642-9.
Murphy P. et al. LATE-BREAKING ABSTRACT: Improving admission free survival with home mechanical ventilation (HMV) and home oxygen therapy (HOT) following life threatening COPD exacerbations: HOT-HMV UK Trial NCT00990132. Eur Respir J 2016; 48: Suppl. 60, 3527
* World Health Organization. “Chronic respiratory diseases: Burden of COPD” Who.int. https://www.who.int/data/gho/publications/world-health-statistics (accessed November 9, 2015)